Movember is a key month for raising awareness of prostate cancer and other key men’s health issues
In a recent fascinating talk in recognition of Movember, Professor Sooriakumaran, one of Thrive4Life’s expert key health speakers, talked about prostate cancer and the importance of regular screening and early treatment.
“You can’t wait for blood in the urine and can’t wait for water-works symptoms, before you look for prostate cancer. The main risk factors are age, genetics, and ethnicity – you can’t stop yourself getting older, you can’t change your family history, and you can’t change your race. So the only thing you can do is to make sure you get yourself tested and screened.”
Professor Prasanna Sooriakumaran

Professor Prasanna Sooriakumaran
Professor of Urology at the Cleveland Clinic Levin College of Medicine, and the Urology Lead at the Cleveland Clinic London.
Introduction
November is traditionally Men’s Health Awareness Month in the UK: sponsored runs are organised, moustaches grown, and men’s health becomes the focus of many a conversation. Magazines, newspapers, and individuals on social media all share information and (often moving) personal stories in a friendly and open fashion, and there can be no doubt that, recently, each year has offered a proliferation of data on a growing number of men’s health topics.
The attention surrounding ‘Movember’ (as Men’s Health Awareness Month is commonly known) is rooted in themes that bear enormous significance for individuals and institutions, with topics such as prostate cancer, testicular cancer, and suicide often taking centre stage.
In this article, we shine a spotlight on prostate cancer, which accounts for 14% of male cancer deaths in the UK. Frequently passing undetected until it’s too late, prostate cancer needs to be tested for proactively. If appropriate measures are taken early enough, survival rates for prostate cancer are higher than they are for many other cancers: 95 out of 100 men with prostate cancer will survive for 5 years or more if the cancer is caught before it spreads to the rest of the body.
Some quick stats…
- In the UK, around 12,000 men die of prostate cancer each year. That’s approximately 33 deaths per day, or one death every 45 minutes.[1]
- Prostate cancer is the second-largest cancer-related cause of death in both the UK and the US.[2]
- Approximately 34,500 men die of prostate cancer each year in the US.[3] That’s more than 94 deaths each day, or one death every 15 minutes.
- Sometimes referred to as a ‘disease of older men’, around 75% of cases of prostate cancer are diagnosed in men over the age of 65.
- The main risk factors for prostate cancer are genes, ethnicity, and age; however, there is also some evidence that being overweight can raise the risk of prostate cancer.[4]
What is the prostate?
The prostate can be found between the rectum and the bladder. It forms an important part of the male reproductive system, producing a fluid component of semen. Typically the size of a walnut, the prostate can grow enlarged with age; this places pressure on the urethra and restricts urine flow, causing ‘waterwork’ symptoms (i.e. difficulties peeing) usually seen in older men.
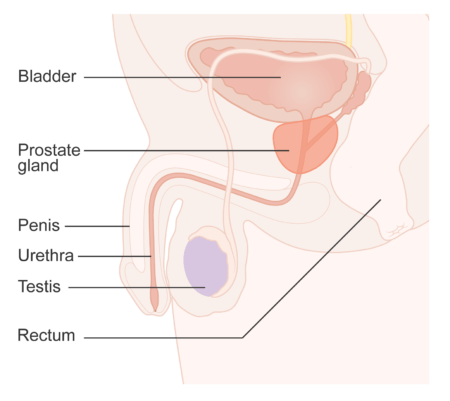
Diagram showing the position of the prostate. [Cancer Research UK, Creative Commons license CC BY-SA 4.0]
What is prostate cancer?
Prostate cancer refers to a cancer that starts in the prostate. If not cured, it can spread to other parts of the body, usually the:
- bones
- lymph nodes
- lungs
- liver.[5]
This is called ‘prostate cancer metastasis’. Once the cancer has spread, the chances of survival decrease dramatically.
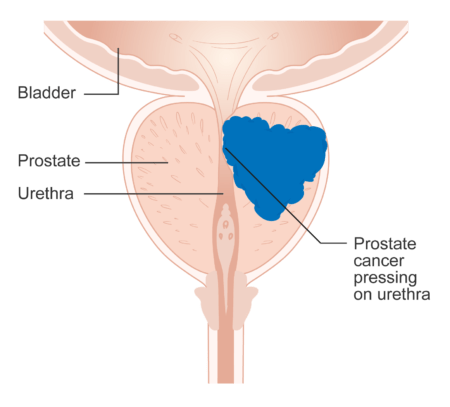
Diagram showing prostate cancer pressing on the urethra [Cancer Research UK, Creative Commons license CC BY-SA 4.0]
What are the symptoms of prostate cancer?
Symptoms such as an increased need to urinate, as well as greater difficulty in doing so, are commonly associated with prostate cancer. However, although these symptoms often are linked to the prostate, they are usually indicative of a benign growth (called benign prostatic hyperplasia), not a cancerous one. Prostate cancer is, in fact, symptomless, and therefore often passes undetected until it has reached a later stage.
Catching the cancer at an early stage is crucial – and can only reliably be done through screening.
Who is most at risk?
Statistics show that 1 in 8 men in the UK will be diagnosed with prostate cancer in their lifetime, but not everyone carries the same risk of prostate cancer.
Other than age (most cases are in men over the age of 50), the most significant known risk factor for prostate cancer is genetic inheritance. A man with a first-degree relative (i.e. brother or father) who has had prostate cancer has a doubled risk of getting prostate cancer.
Ethnicity is another factor that raises the risks of getting prostate cancer. Certain ethnic groups, such as Afro-Caribbean and Ashkenazi Jewish men, who carry a doubled risk of getting prostate cancer.
Thus, men with higher risks of prostate cancer need to test for it more frequently, as early diagnosis can increase the chances of survival. An Afro-Caribbean man whose father or brother has had prostate cancer has an approximately 50% risk of suffering from prostate cancer in his own lifetime.
As Professor Sooriakumaran puts it, “you can’t stop yourself getting older, you can’t change your family history, and you can’t change your race. So the only thing you can do as a man with risk factors is to make sure you get yourself tested and screened”.
How do you screen for prostate cancer?
There are two ways of carrying out initial screening for prostate cancer: through a blood test (PSA) or a rectal exam.
- As part of its role in the male reproductive system, the prostate produces prostate-specific antigen (PSA), a protein which liquifies semen, allowing the sperm to swim more fluidly. A PSA test – or Prostate Specific Antigen test – typically can be performed in about 1 minute, and involves taking a blood sample. PSA tests have attracted a degree of controversy, largely due to suggestions that their unreliability leads to inaccurate diagnoses and unnecessary treatment. Indeed, because of the press reputation of PSA tests, a large number of GPs hesitate or refuse to recommend them.However, part of that hesitation may have to do with how difficult it is to interpret PSA tests: due to their sensitivity, these tests require an expert to interpret them, and are reliable when correctly interpreted in a post-surgery setting. According to Professor Sooriakumaran, compared to tumour markers for other cancers, the PSA is the best cancer-specific antigen test on the market.
- The second method of screening for prostate cancer is the rectal exam. This involves the doctor inserting a lubricated, gloved finger into the patient’s rectum, to feel for unusual signs in the prostate. The exam takes very little time to complete, and usually causes little discomfort to the patient.
What if further testing is required?
If the initial tests are a cause for concern, the doctor will refer the patient for more testing at the hospital. As well as further PSA and rectal examinations, the patient may be offered the following:
- MRI scans. Magnetic Resonance Imaging scans typically take 30-45 minutes to complete, and show up abnormalities in the prostate. Although a helpful scan, MRI doesn’t provide all of the information required to know whether the prostate is affected by cancer or not. About 10% of prostate cancers won’t be seen on an MRI scan.
- Transperineal biopsy of the prostate. Transperineal biopsies involve taking a sample of the prostate by inserting a needle through the perineum. This allows doctors to assess the severity of the cancer down a microscope, and assign a Gleason score. (The Gleason score is a prostate cancer-specific score which describes the severity of the cancer. Although the scale theoretically runs from 2-10, only 6-10 are commonly used, with 6 being the lowest-grade cancer).
How is prostate cancer treated?
Once it has been determined that a person has prostate cancer, there is a variety of different treatments available to them, the most common (and the most tried-and-tested) being radiotherapy and surgery.
- Surgery is usually used for men up to the age of 75, and involves the removal of the prostate, sometimes with the help of robotic surgery.
- For men who are not fit for surgery, radiotherapy can be used.
Additionally, there are experimental and unproven treatments, such as ultrasound, laser, freezing and cryotherapy. However, these have not been found to yield long-term results, with the cancer typically returning after treatment.
What are the survival rates for prostate cancer?
An individual’s chances of survival of prostate cancer will depend on a number of factors, and cannot be reliably predicted. However, sufficient data exists to break survival rates down into a number of categories:
Duration:
- 95% of men with prostate cancer will live for 1 year or more.
- 85% of men with prostate cancer will live for 5 years or more.
- Almost 80% will survive for 10 years or more.
Stage:
- Stages 1&2: almost 100% of patients will survive stage 1 and stage 2 prostate cancer, in which the cancer is confined to just half of the prostrate or less.
- Stage 3: approximately 95% of patients will survive their prostate cancer for 5 years or more if the cancer is caught in stage 3 – that is, when the cancer has broken through the prostate gland’s covering but not spread further.
- Stage 4: only around 50% of men with stage 4 cancer (when it has spread to nearby bones, organs or lymph nodes) will survive longer than 5 years.[6]
These statistics show the significantly increased rates of survival that come with early diagnosis.
Summary
Professor Prasanna Sooriakumaran ended his extremely informative talk by summarising that prostate cancer is an extremely common type of cancer among men. Certain factors, such as age, ethnicity and genetics, make it a higher-risk disease for some than for others. Due to the lack of symptoms that accompany prostate cancer, testing is necessary to spot it and intervene at an early enough stage to make a difference. A variety of treatments exist, with radiotherapy and surgery being the most common and effective.
Interested in having a professional speaker talk to your employees?
Our educational livestreamed talks connect your employees to leading health and wellbeing experts with the aim of empowering them to lead healthier and more productive work lives.
Find out more about our educational talks and webinars, or get in touch to arrange access for your staff.
References
- https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer
- https://www.cancer.net/cancer-types/prostate-cancer/statistics
- https://zerocancer.org/learn/about-prostate-cancer/facts-statistics/
- https://www.wcrf-uk.org/cancer-types/prostate-cancer/?gclid=EAIaIQobChMIwrXt2PjB-wIVTO7tCh26mwiREAAYASAAEgKwGvD_BwE
- https://www.mayoclinic.org/diseases-conditions/prostate-cancer/expert-answers/prostate-cancer-metastasis/faq-20058270
- https://www.cancerresearchuk.org/about-cancer/prostate-cancer/survival
- Men’s Health Webinar by Professor Sooriakumaran 17th November 2022 – www.thrive4life.co.uk/event/mens-health-webinar-movember-2022/











